Imagine you’re driving on a winding road, trying to reach your destination. You’re confident in your skills and knowledge of the route, but suddenly, you encounter a roadblock. Your progress is halted, and you’re left wondering how to navigate around this obstacle.
Similar to this scenario, mastering the revenue cycle in healthcare can be a complex journey. It requires a deep understanding of the key insights into Revenue Cycle Management (RCM) to ensure smooth operations and financial success for healthcare organizations.
In this discussion, we will explore the crucial components of RCM, strategies for optimization, common challenges faced, and best practices to keep the revenue flowing seamlessly.
So, buckle up and get ready to uncover the secrets of mastering the revenue cycle.
Understanding the Revenue Cycle

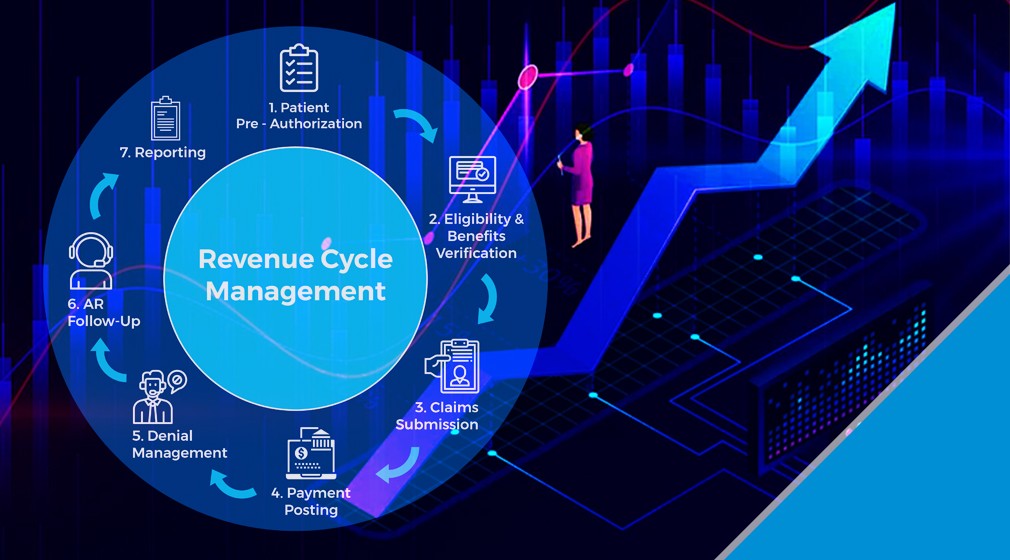
To truly master the revenue cycle, it’s essential to have a comprehensive understanding of its intricacies and processes. The revenue cycle management process refers to the steps involved in capturing, processing, and collecting revenue from patient services. It encompasses various activities, such as patient registration, insurance verification, charge capture, claims submission, and payment posting. Each stage is interconnected and plays a crucial role in ensuring a smooth flow of revenue.
To measure the effectiveness of the revenue cycle, organizations rely on revenue cycle performance metrics. These metrics provide insights into the financial health of the healthcare facility and help identify areas for improvement. Key performance indicators (KPIs) such as Days in Accounts Receivable (DAR), Clean Claims Rate (CCR), and Collection Rate are commonly used to assess the revenue cycle’s efficiency.
Understanding the revenue cycle and its associated processes is vital for healthcare organizations to optimize revenue generation. By closely monitoring performance metrics, organizations can identify bottlenecks, streamline processes, and enhance revenue collection. It’s crucial to implement robust revenue cycle management strategies and leverage technology solutions to improve revenue cycle performance.
Key Components of RCM
The key components of revenue cycle management (RCM) include patient registration, insurance verification, charge capture, claims submission, and payment posting. Each of these components plays a crucial role in ensuring the smooth flow of revenue within a healthcare organization.
Patient registration is the first step in the revenue cycle and involves gathering accurate demographic and insurance information from patients. This data is vital for subsequent steps in RCM, such as insurance verification. Insurance verification involves confirming the patient’s coverage and eligibility, ensuring that claims will be paid in a timely manner.
Charge capture is the process of capturing and documenting all billable services provided to patients. This step requires attention to detail to ensure that no services are missed or undercoded.
Claims submission is the next step, where the documented services are transformed into claims and submitted to insurance payers. Accuracy and compliance with billing guidelines are essential to avoid claim denials and delays in reimbursement.
Payment posting is the final component, where payments received from insurance payers and patients are recorded and reconciled with the corresponding claims. This step involves careful tracking of payments and identification of any discrepancies for follow-up and resolution.
Strategies for Revenue Cycle Optimization

Implementing effective strategies is essential for optimizing the revenue cycle in healthcare organizations.
To improve revenue cycle efficiency, healthcare organizations should focus on revenue cycle analysis to identify areas for improvement and implement targeted solutions.
One strategy is to streamline the registration process by implementing electronic data capture systems and automating eligibility verification. This reduces errors and delays, ensuring accurate and prompt billing.
Another strategy is to improve documentation and coding practices to ensure proper reimbursement. Implementing regular audits and providing training to staff can help identify and address any coding or documentation deficiencies.
Additionally, leveraging technology such as revenue cycle management software can help automate and streamline the billing and collections process, reducing manual errors and improving overall efficiency.
It’s also important to establish clear communication and collaboration between billing and clinical departments to address any issues or discrepancies promptly.
Common Challenges in RCM
As healthcare organizations strive to optimize their revenue cycle, they often encounter common challenges that hinder their financial performance and revenue generation. Two significant challenges in revenue cycle management (RCM) are reimbursement delays and denials management.
Reimbursement delays occur when healthcare organizations experience delays in receiving payments for the services provided. These delays can be caused by various factors, such as incomplete or inaccurate documentation, coding errors, and slow processing by payers. To address this challenge, organizations should implement strategies to streamline their billing and coding processes, improve documentation accuracy, and establish effective communication channels with payers to expedite the reimbursement process.
Denials management is another common challenge that impacts revenue cycle performance. Denials occur when payers reject claims for various reasons, such as coding errors, lack of medical necessity, or missing documentation. To effectively manage denials, healthcare organizations should implement robust denial management processes, including regular monitoring and analysis of denial trends, proactive identification of root causes, and timely resubmission of denied claims with the necessary corrections.
Best Practices for a Smooth Revenue Flow

To ensure a smooth revenue flow, healthcare organizations should adopt efficient practices for maximizing revenue generation and minimizing financial disruptions.
Streamlining billing processes is crucial in achieving this goal. By implementing automated billing systems, organizations can reduce manual errors and improve the accuracy of claims submission. This ensures that claims are processed quickly and accurately, leading to faster reimbursements.
Another best practice is to maximize reimbursement opportunities. This involves staying up-to-date with coding and documentation guidelines to ensure accurate and complete documentation of patient encounters. By properly coding and documenting services provided, healthcare organizations can optimize reimbursement and avoid denials or underpayments.
Regularly monitoring key performance indicators (KPIs) is also essential. This allows organizations to identify any bottlenecks or inefficiencies in the revenue cycle process and take appropriate action to address them. By closely tracking metrics such as days in accounts receivable and denial rates, organizations can proactively identify areas for improvement and implement strategies to enhance revenue flow.
Moreover, implementing effective revenue cycle management software can streamline the entire revenue cycle process. This software automates tasks such as patient registration, claims submission, and payment posting, reducing manual effort and increasing efficiency. It also provides real-time analytics and reporting, enabling organizations to make data-driven decisions and optimize revenue generation.
Frequently Asked Questions
How Can Healthcare Organizations Ensure Patient Data Security During the Revenue Cycle Process?
To ensure patient data security during the revenue cycle process, you should implement data encryption and cybersecurity measures. These measures will protect sensitive information and minimize the risk of unauthorized access or data breaches.
What Are the Potential Risks and Consequences of Not Implementing Effective Revenue Cycle Management Strategies?
Without effective revenue cycle management strategies, you risk low patient engagement, leading to decreased financial reimbursement. This can result in delayed payments, increased denials, and overall financial instability for your healthcare organization.
Are There Any Specific Regulations or Compliance Requirements That Healthcare Providers Need to Consider When Optimizing Their Revenue Cycle?
When optimizing your revenue cycle, it’s crucial to consider specific regulations and compliance requirements. These include healthcare reimbursement guidelines and regulatory compliance standards that ensure accurate billing and coding practices.
How Can Technology and Automation Be Leveraged to Streamline and Improve the Revenue Cycle Management Process?
You can streamline and improve your revenue cycle management process by leveraging technology integration and implementing automation. These tools can help optimize workflows, reduce errors, and increase efficiency in managing financial transactions and claims processing.
What Are Some Key Performance Indicators (Kpis) That Healthcare Organizations Should Track to Monitor the Effectiveness of Their Revenue Cycle Management Efforts?
To monitor the effectiveness of your revenue cycle management efforts, healthcare organizations should track key performance indicators (KPIs) such as patient satisfaction and financial performance. These metrics provide insight into the success of your RCM strategies.